sug_97
-
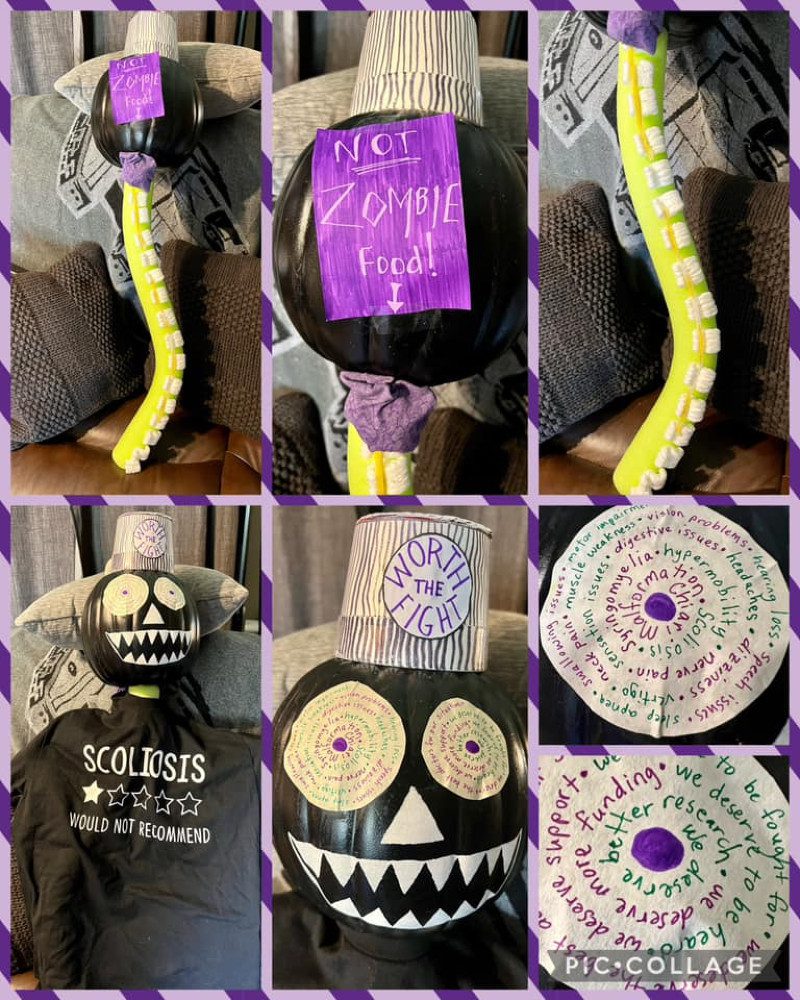
Awareness Pumpkin 2023 Contestant 2: Ethan and Amy D (mom)
Voting is now closed.
-

Awareness Pumpkin 2023 Contestant 1: Haley E.
Voting is now closed.
-
September Is Chiari Awareness Month
It’s hard having a chronic illness that isn’t all that understood. As patients, we have to fight on absolutely every level! Before diagnoses, we fight for someone to hear us when: Around diagnoses, we fight to: When our doctors continue to dismiss our symptoms, we need our friends and families to understand:
-
![The Important Questions to Ask Your Neurosurgeon [Revised]](https://dev.chiaribridges.org/wp-content/uploads/2023/09/MRI-doctor_AS505903501.jpg)
The Important Questions to Ask Your Neurosurgeon [Revised]
Most Chiarians go to see a surgeon with an expectation of them being knowledgeable in their field. However, while they might be a neurosurgeon, their knowledge of Chiari and its comorbid/pathological conditions might not rank high in their practice. Make the most of your initial appointment by interviewing them and what they really know about…
-

Obtaining Your MRIs on Disk
Hospitals and imaging centers in the United States are required to give you a copy of your imaging if you request it. Many hospitals and imaging centers will give a copy of your MRI on disk or flash drive immediately after your appointment, but they do this as a courtesy and not as a requirement.…
-

Understanding Your Head and Neck Pain
You Might Have More Than A Migraine If… High-Pressure Headaches Those that suffer from high pressure tend to feel pressure behind the eyes (often mistaken for sinus headaches) and report feeling like their “head is going to explode” from the pressure. High-pressure headaches are generally characterized by being worse when laying down – often awaking…
-
Christmas Presence
Making homemade stockings and cutting flowers for wreaths. Baking treats and devouring them with hot cocoa by the tree that we spent hours decorating. Shopping for just the right gifts and wrapping them meticulously, so those I love know just how special they are. I remember all the traditions that we did together as a…
-
Guidelines for Nonprofessional Opinions (NPOs)
If you decide to post your MRIs for Nonprofessional Opinions (NPOs) at WTF, please make sure that your post/images adhere to the following guidelines. Requests that do not meet our guidelines will be removed by an admin. PLEASE MAINTAIN 100% PRIVACY TOWARDS THOSE TRYING TO HELP YOU OR SOMEONE ELSE. We have very strict privacy rules…
-

Nonprofessional Opinion (NPO) Request Form
The Nonprofessional Opinion (NPO) Request Form is required for all formal requests with the Admin Think Tank (ATT) – no exceptions.
-

