As I sit down to update my journey, I am crushed that we’re still figuring things out (and nothing really was as I was initially told it would be), yet at the same time, I’m so thankful that we’re continuing to figure things out. Nobody should have to fight a fight like this (every symptom, every diagnosis), but all of this just increases my resolve to change it before anyone else in my family (or yours) is having to fight it! What we fail to change in our generation, our children and their children will face in theirs!
Looking back, I have always had symptoms of Ehlers-Danlos Syndrome (EDS). As a child, I was in the school nurse’s office for stomach problems at least once a week. I was “double-jointed” and my friends always asked me to do maneuvers that I thought everyone should really be able to do if they tried. I was athletic early on, a tom-boy. I particularly loved playing softball (or baseball with tennis balls was the absolute best), but my ankles rolled when I started to run. Despite the fact that I was the only player that twisted their ankle multiple times in every game, I didn’t think there was really anything abnormal about me. Later, as an adult, I had repeated miscarriages and complications in all of my pregnancies, but the doctors conveniently came up with different explanations for each “rare occurrence.” It couldn’t possibly be all those rare mishaps, but EDS explained it all.
My mother passed away from a brain aneurysm the day after my 18th birthday. She was just 37 years old when she died. As a child she had a lazy eye and scoliosis of the spine, so an eye patch and back brace were a normal part of her childhood attire. She suffered from migraines throughout her adulthood, but nothing was more tale-telling than reading her journal after she passed, with multiple entries about repeated headaches and neck pain. Decades after her death, my maternal grandmother (my mother’s mother) developed multiple brain aneurysms over the course of a decade. Each time one appeared, she had it filled with titanium coils. I always admired her fight for life.

The first headaches that I remember started immediately after giving birth to my first son in 1992. It was a cesarean section at an Army hospital in Fort Ord, California. Instead of an epidural, they gave me three spinal injections to numb me from the chest down. At my postpartum check-up, I complained of daily headaches when upright. My primary care doctor ordered a CT scan, but because it was just a few years after my mom had died they looked only for brain aneurysms and found none. I was still having those orthostatic headaches six months later.

The Accident that Shook Everything
In 2000, I was a Bible College student and stay-at-home mom of three happy and active children (ages 8, 5, and 2). One September night, I was in a car accident that changed all of our lives. My neck was never the same again. My initial symptoms were head/neck pain, but all radiology reports indicated that everything was “unremarkable.” I tried everything they offered to me: rest, acupuncture, acupressure, steroid injections, osteopathic and chiropractic care, nerve stimulation units, physical therapy, pain meds, etc. Nothing worked long-term. Then in 2005, my neurological problems started intensifying. I began having bouts of partial paralysis in my legs and hands. I would just wake up one morning and out of the blue, I would have no fine motor skills. I would wake up feeling as though I had no thigh muscles to support me when I walked or tried to step up a step, and I had difficulty coordinating my footsteps. My primary care doctor at the time did blood tests and concluded that my “potassium level was on the low side of normal, so it must have been from potassium shock,” and he thought that no other tests were warranted. I started having vertigo whenever I was at any elevated height, even just a step or two up, like my brain couldn’t figure out how to balance with visual changes in height (I’d take a step up or down like the step was much higher or lower than it actually was). I also started having noticeable memory issues and intermittent trouble processing information. They tested to see if I was having small seizures in my sleep. When that was ruled out, they referred me to the memory clinic for further cognitive testing. They had no cognitive baseline to compare my results to, but said that I “tested higher than 89% of the population, so I should be happy,” and that I should just try reducing stress in case it was stress-related. They didn’t understand that it didn’t matter to me “how I compared to others.” I was only 34 years old and something was very wrong with me; I wanted answers that had nothing to do with the general population. In 2006, my eyes started twitching all day, every day, until the muscles just wore out and I could no longer hold them open completely. Oddly, one of my college professors inquired about my eyes and recommended that I have it investigated because it “could be neurological in origin.” When I did talk to my doctor about it, he saw the recommendations of the Memory Clinic and attributed it to stress as well, without any testing.

My Chiari Diagnosis
Finally, in 2010, ten years after the car accident, another MRI was done at my insistence to check for aneurysms once again (because I still was having excruciating head/neck pain and trouble holding my head up). I received an email from my primary care doctor that they found a cause of all of my symptoms. It was a condition called Chiari Malformation and the neurosurgery department would be contacting me to make an appointment. The neurosurgeon (who became my neurosurgeon) checked through my MRIs and said that the Chiari Malformation was evident on my first MRI after the accident ten years earlier. I was told that it was congenital and that it is commonly believed to be a result of prenatal drug use or lack of proper prenatal care (which was devastating to hear, but not all that unlikely as I was born in 1971. It also ended up being very wrong “textbook information” that they tell us all). Desperate for a measure of relief, I underwent a full decompression surgery a few weeks later. Missing the fact that part of my brain was in my spinal canal was 100% the hospital’s fault, but in hindsight, I really wish that I had done more research before surgery. I had comorbid conditions (many of which my doctors hadn’t even heard of, didn’t fully understand, and more importantly, they didn’t know the connection between these comorbids and my herniated tonsils). Initially, I felt quite a bit better. The release of pressure in my head helped my headaches. It was short lived though. Those undiagnosed comorbids caused my decompression to ultimately fail, although it all unfolded over several years.

Post-op Complication: Pseudomeningocele
When I was released from the hospital following decompression surgery, I was instructed not to lift, push, or pull anything for two weeks so that my dura patch would have a chance to adhere. The problem was, I could feel fluid squeezing out of the patch far beyond that two-week limit. I developed a pseudomeningocele (blue box above), which can be normal immediately after surgery before the dura adheres, but as long as there is no active leak, the body should absorb the fluid and the pseudomeningocele should quickly resolve. My neurosurgeon tapped some of the fluid out with a syringe twice and we waited patiently to see if it would subside on its own. It did not subside and in December 2012 (just over two years post-decompression), I developed acute vertigo. Everything was spinning and rocking, non-stop. It didn’t matter if my eyes were open or closed. I was waking up vomiting in my sleep from the dizziness. I couldn’t walk at all without falling hard to my right. I had no sense of balance at all and it didn’t just come and go, it was constant. Another MRI was done and it showed that my cerebellum was absorbing the fluid from the pseudomeningocele (so the cerebrospinal fluid was inside my brain, not just surrounding it; see light blue circle in image above). The decision was made to put in a subgaleo-peritoneal shunt (SP shunt), which runs from the pseudomeningocele to my peritoneum. They expected that it might take up to six months to fully drain from my cerebellum, but I woke up from the anesthesia with no signs of vertigo. I believe this surgery saved my life, but as with all shunts (especially amongst those with EDS, which I had not yet been diagnosed with), the shunt was destined to cause problems all by itself.

My Many Shunt Revisions
In April 2013, an unrelated CT Scan revealed that my shunt was no longer in my peritoneum. My NS scheduled for a general surgeon to “tie in” my shunt so it would not happen again (surgery #3). We went several months without complication until that November. The tied in shunt pulled out of my peritoneum again (it was excruciating). Hoping gravity would help in the matter, my NS did an incision just under my right rib cage and dropped it down into my peritoneum (surgery #4). Shortly thereafter, radiologist reports started showing a concern for the location of my brain and I was diagnosed with “Sagging Brain Syndrome.” So my six-week post-op appointment (which my NS did faithfully after every surgery) became my pre-op appointment for my 5th related surgery. This time a non-adjustable valve was attached to the shunt (at my chest) in hopes that by slowing down the amount of CSF being drained by the shunt, my head could retain more fluid and my brain could once again lift and become buoyant. Five months later I developed a hernia and upon closer examination (during surgery), it was found that my peritoneum was literally falling apart from all the trauma of the shunts; so my hernia removal surgery became a reconstruction surgery where my abdominal wall was pulled together with mesh, while carefully ensuring that the shunt didn’t come out (surgery #6). The shunt never moved again. As my brain continued to sag, the choice was made to replace the valve with an adjustable valve and in November of that same year, I was having surgery #7. The valve was adjusted to its slowest possible setting in hopes of finding a balance where it drained enough to keep the hydrocephalus at bay, yet retain enough CSF to lift my brain and keep it lifted and out of my spinal canal (so we could establish flow to the spinal canal and avoid the possibility of a syrinx).
Diagnosis: Ehlers-Danlos Syndrome
Despite my concerns that I might have a connective tissue issue and being told over-and-over again that I “didn’t look like someone with Ehlers-Danlos Syndrome,” I was finally diagnosed with it in May 2015. After finally finding a neurologist who understood the role that our connective tissues can have in a Chiari Malformation, I was given a referral to a geneticist. It still wasn’t as easy as it should be though. The geneticist did not know much about Chiari or Ehlers-Danlos related conditions (although he didn’t initially admit to that), so I had no idea at that point what was and was not related, and neither did my doctors. I received a call from the geneticist’s assistant and I agreed to send her pictures of my hypermobile maneuvers from the Beighton Scale. I could do all but bend over and put my hands flat on the floor with my knees straight, but I was able to do that when I was younger (and thinner). I was given a 9/9 on the Beighton Scale and was told that he would just mark my chart as diagnosed “hypermobile” and that he didn’t need to see me. I honestly didn’t know any better at this point, but I was about to learn something very important. I sat there thinking about what this “hypermobile” diagnosis would mean for me and decided to look more into EDS for myself. I read about the high risk of aneurysms, organ tearing, miscarriages, etc. and I was back on the phone with that assistant within twenty minutes. She asked if she could call me back, and within the hour the geneticist had decided that he needed to see me. He set up an appointment with me within twenty-four hours and asked if it was okay if he had a few others (doctors and medical students) there as well, since they’re a training hospital and they “don’t really come across patients with Ehlers-Danlos” (he should have told me that from the beginning). I agreed. Despite his lack of knowledge on EDS related comorbidities, he did know exactly where on my body to look for characteristics of EDS (all of which I thought I didn’t have). For instance, my skin isn’t unusually elastic, except in my upper arms and upper thighs. My skin isn’t translucent (I’m olive complected), except for on my breasts, back, and inner forearms. My skin isn’t unusually soft, except on my back. Now concerned that I might have Vascular Type EDS (vEDS), he decided to have me tested for that. The test was easy on my part but expensive on theirs. They drew blood and had it refrigerated and shipped to a lab in Washington state. It took thirty days for them to make sure that there was no mutation in my COL3A1 (collagen 3; alpha 1) gene, which has a median mortality age of 48. Initially, I felt devastated, since I was already 44. I decided that I hadn’t fought through all that I had, to only live a few more years. Thirty days later, the test came back indicating that I didn’t have vEDS and by default, I was diagnosed with Hypermobility Type EDS (hEDS). I was relieved, but the geneticist assured me that I still needed to be cautious. Since EDS symptoms are known to cross the type boundaries, and we already knew that vascular complications ran in the family (with the aneurysms) and with me personally (my peritoneum tearing), it technically made me “hEDS with vEDS crossover symptoms” and I’d probably have to explain that to my doctors for the rest of my life, so they remain aware of my potential to have additional vascular problems.

My Poor Mess of a Neck
The electric shock feeling in my spine (Lhermitte’s Sign) that I’d had intermittently for years, became an all-day, everyday thing, and much stronger in intensity. The MRI revealed that the herniated disc I had between my C3/4 was getting worse. The disc was removed with cadaver put in its place and the discs were fused together. My 8th surgery (ACDF = Anterior Cervical Discectomy and Fusion) wasn’t related to Chiari, but it was related to the EDS. We knew that my cervical spine was really bad from the beginning, but it got worse. I am now actually diagnosed with Degenerative Disc Disease in all three levels of my spine, but my neck has by far taken the brunt of it all. The ACDF, while 100% necessary, compromised the discs adjacent to it, and every disc from C4-7 is either bulging or herniated (Subaxial (cervical) Instability), so additional surgeries are likely to be needed.
Learning to Advocate for Myself
Over the past several years I have become an enthusiast of Chiari related research and MRIs (out of medical necessity more than anything). It became apparent to me that I absolutely needed to know everything that was going on in my body in case my doctors didn’t. When I first started, I’d print out studies and lay in bed with multiple high-lighters. I had such brain fog that I’d lay there crying at the fact that I was reading and rereading the same paragraphs over again, but I knew that I had to learn it despite how impossible it seemed. I prayed a lot for God to help me with my understanding and He did. I also started looking at the medications I was taking, the supplements I was taking, and what the ideal doses were for me (especially those that would help with inflammation and cognition), and other natural remedies. The first thing that I removed was all of the nerve meds that they had me on for peripheral neuropathy. I was maxed out on Nortriptyline (a tricyclic antidepressant) and almost maxed on Gabapentin (both of which had caused me to gain an incredible amount of weight over the years). When I informed my primary care doctor that I wanted to go off of them all, he thought it was a bad idea because of the severity of my neuropathy. I insisted though and asked him to help me to wean myself off of both of them in healthy intervals, and let’s “just see.” With the first down-dose, I physically felt a reduction in inflammation. It took me many months to wean off and get them out of my system, but in hindsight, I think this was the single best decision that I could have made. The longer I was on supplements instead of the nerve meds, the more my brain-fog improved, and I now believe that I have regained all that I’ve lost cognitively and then some.

Syringobulbia
In 2016, I was reviewing some of my old MRIs and I saw a large CSF filled hole in my lower medulla oblongata (lower brainstem). It was obvious in all MRI series since 2015, yet I was told that all was stable. After researching it, I asked my neurologist to take a look and see if it could be Syringobulbia. She referred my question to my neurosurgeon and he confirmed that I had an 11mm cyst in my brain stem. This type of cyst happens when there is a blockage of cerebrospinal fluid and is most frequent when the brain stem is also herniated below the foramen magnum (Chiari 1.5). It explained a lot of the problems that I was having, that we had thought to be unrelated. For instance, and I had a decreased sensitivity to temperature for years, never feeling hot or cold; and never having the automatic reactions that I should have had in response to temperature, like sweating and shivering. I could comfortably be outside in heat above 100° without breaking a sweat, or be outside in shorts and a tank-top when it was a chilly 30° morning without ever shivering. I also developed tachycardia and I am now medicated to keep my heart rate down to a safe level. My neurosurgeon ordered a new MRI in April 2017. The size of the syrinx had decreased to 9mm but was draining down my spinal cord forming an additional syrinx (Syringomyelia).

Consulting a Specialist
After all that I had been through in my fight, in April 2017, I decided to pay out of the pocket and have an online consultation with a Chiari Specialist in New York, who specializes in Chiari with EDS (the best $300 that I’ve spent in my fight). I sent him my pertinent medical records and copies of my MRIs in advance, wanting to find out what my doctor did right, and what he did wrong; and what course of action should be taken at that point. My expectation was that he would give me reasons why I should go to New York to see him, but that’s not at all what he told me. He told me what my doctor did right and that he didn’t disagree with the course of action that my neurosurgeon wanted to take. He said that my brain had sagged as low as it really could, but that since my high/low pressures had balanced out, and I was feeling better than I had in years, my syringes really should dictate our next course of action.
In March 2018, following an exceptional year (at least where my head and neck are concerned) new imaging was done. My neurosurgeon asked me to come in to review it. It gave me a chance to tell him about the specialist’s opinions. My MRI showed that the Syringobulbia had decreased another 2mm. I asked him what that meant for the cervical syrinx, and that had almost completely disappeared. I asked him to go back to my images and correct me if I was wrong, but “the only reason that a syrinx (in either location) would dissipate like that was if I was finally getting CSF flow down my canal (despite my severe brain sag).” He agreed and I think he was a little surprised to see me think on my feet and figure that out in front of him (where I wasn’t having to ask anyone or look it up). He also confirmed that I had an Acquired Chiari, secondary to Intracranial Hypertension. He applauded me for learning all that I had and said that he wished that he had checked my pressures before decompressing me, as it may have changed the course of action that we had taken. And we agreed to wait a year and see where the syringes (syrinxes) are. As I left his office that day, I felt such a sense of relief, that we were finally getting CSF flow like the decompression in 2010 was meant to do.
My Extensive Epidural CSF Collection
In 2022, my neurosurgeon contacted me telling me that he was retiring and he’d like to have one last MRI of my entire spine (he added the brain to the request at my request). Unbeknownst to me, he ordered a CSF Leak Protocol, which consists of less slices, but they’re specifically looking for leaks. The images showed an “extensive extradural CSF collection from C7-L4, consistent with a CSF Leak and probable dural tear or CSF Venous Fistula.” They followed up with a Dynamic CT Myelogram. A Dynamic is different than a regular CT Myelogram, as they do it over 2-3 days, and they insert the contrast little by little into my spinal canal, and watch carefully for it to leave the spinal canal. CSF leaks and dural tears aren’t uncommon amongst Ehlers-Danlos patients, and usually happen in the front or back of the canal. CSF Venous Fistulas on the other hand are a much newer phenomenon, and they usually happen on the sides of the canal (more often on the right side). After two days of grueling tests, they found no active leaks or evidence of fistulas and surmised that what they saw on the MRIs to be “residual artifacts” from a leak that I had in the past… a leak that could have pulled my brain down into my spinal canal in the first place.

It’s been a long road, hard road. I still battle inflammation and I’m definitely not done with surgeries. Eventually, I will need a ventriculoatrial (VA) shunt to hopefully resolve my high-pressure issues and enable us to remove my over-draining SP shunt that is making my brain sag. But for right now, I’m just enjoying feeling so much better! I praise God every step of the way, as I know that He’s there making a way out of no way. I have no idea why He took so long or why others haven’t seen the same results (because He loves them as much as He loves me), but I don’t have to have all the answers. I’ll just praise Him through the course of my journey, as He’s never let me go through it alone!
*I dedicate this story to my family: John (husband), Ron (dad), Johnathan (son), MyKaella (daughter), Jojo (son) and my daughters-in-law, Violet and Sarah. Thank you all for all your help and for standing and kneeling beside me throughout my entire ordeal. You’ve been there for me and loved me through this long haul and I praise God for each and every one of you.
Originally written in 2018. Updated April 2022.
![The Michelle Cole Story – A Chiari Warrior’s Journey [UPDATED]](https://dev.chiaribridges.org/wp-content/uploads/2018/12/DSC07853t.jpg)

 Colton had just finished his Chiari Decompression. He was headache free and doing great! His neurosurgeon came to me and said, “This is a genetic disorder and Emmalyn should be checked.” Two weeks later I took Emmalyn into the Chicago area to be sedated for her first MRI of the brain and spine. Three hours later I met Emmalyn in recovery where she came out of anesthesia smiling. Emmalyn was three years old and asymptomatic, not even a headache. Colton’s neurosurgeon called me the next day and let me know that she was only 5mm herniated, but in the spinal MRI, she had two separate syrinxes. A smaller one in her cervical spine and a very large one in her thoracic spine. Her opinion was to decompress Emmalyn right away as she was very concerned about the two syringes and explained, “With the decompression, it should allow the syringes to dissipate.” So, we scheduled her first decompression for two-weeks later, on July 31st, 2012. Emmalyn went through her first decompression like a champ and was released from hospital after three days. This is when Emmalyn’s headaches started. It seemed like once a day she would be getting a headache. Two weeks into recovery Emmalyn was sitting in a chair and said that she felt sick to her stomach, so she ran into the bathroom, I followed and as she was heaving her head went deeper into the toilet. I picked her up and her eyes darted to the right and she couldn’t talk to me. I immediately called 911. When the paramedics arrived, they swept her from my arms and rushed her to the ambulance. They kept her in front of our house in the ambulance for about ten minutes before they came and told me she was having a seizure; they didn’t want to jostle her head, so they called the helicopter. We were told to meet the helicopter at the hospital, which is forty-five minutes away. My husband and I jumped in our van and I don’t think I have ever seen my husband drive so fast; we beat the helicopter there. When the helicopter landed, we were in the ER to greet her when she came off the elevator, and when she did, she was covered in blood and screaming. I looked to the helicopter nurse and she said, “Two minutes before landing she came to and she wanted her mom and pulled out her IV.” She had a forty-five-minute seizure. We are in “small-town,” USA, so the ER did a quick MRI, bloodwork, but no EEG and at the time I didn’t know she should have had one. So, they said she was fine and released her from the hospital. Of course, after speaking with her neurosurgeon the next day she had us in the car to make the five-hour drive for her to be admitted. After three days of tests, they concluded that she had chemical meningitis and put her on medication and anti-seizure meds for six months. Let me tell you that was the scariest time of my life, but Emmalyn took it like a champ. In three months, we had repeat scans, her decompression site looked good, but her syringes didn’t change in size, so we chose to wait and see.
Colton had just finished his Chiari Decompression. He was headache free and doing great! His neurosurgeon came to me and said, “This is a genetic disorder and Emmalyn should be checked.” Two weeks later I took Emmalyn into the Chicago area to be sedated for her first MRI of the brain and spine. Three hours later I met Emmalyn in recovery where she came out of anesthesia smiling. Emmalyn was three years old and asymptomatic, not even a headache. Colton’s neurosurgeon called me the next day and let me know that she was only 5mm herniated, but in the spinal MRI, she had two separate syrinxes. A smaller one in her cervical spine and a very large one in her thoracic spine. Her opinion was to decompress Emmalyn right away as she was very concerned about the two syringes and explained, “With the decompression, it should allow the syringes to dissipate.” So, we scheduled her first decompression for two-weeks later, on July 31st, 2012. Emmalyn went through her first decompression like a champ and was released from hospital after three days. This is when Emmalyn’s headaches started. It seemed like once a day she would be getting a headache. Two weeks into recovery Emmalyn was sitting in a chair and said that she felt sick to her stomach, so she ran into the bathroom, I followed and as she was heaving her head went deeper into the toilet. I picked her up and her eyes darted to the right and she couldn’t talk to me. I immediately called 911. When the paramedics arrived, they swept her from my arms and rushed her to the ambulance. They kept her in front of our house in the ambulance for about ten minutes before they came and told me she was having a seizure; they didn’t want to jostle her head, so they called the helicopter. We were told to meet the helicopter at the hospital, which is forty-five minutes away. My husband and I jumped in our van and I don’t think I have ever seen my husband drive so fast; we beat the helicopter there. When the helicopter landed, we were in the ER to greet her when she came off the elevator, and when she did, she was covered in blood and screaming. I looked to the helicopter nurse and she said, “Two minutes before landing she came to and she wanted her mom and pulled out her IV.” She had a forty-five-minute seizure. We are in “small-town,” USA, so the ER did a quick MRI, bloodwork, but no EEG and at the time I didn’t know she should have had one. So, they said she was fine and released her from the hospital. Of course, after speaking with her neurosurgeon the next day she had us in the car to make the five-hour drive for her to be admitted. After three days of tests, they concluded that she had chemical meningitis and put her on medication and anti-seizure meds for six months. Let me tell you that was the scariest time of my life, but Emmalyn took it like a champ. In three months, we had repeat scans, her decompression site looked good, but her syringes didn’t change in size, so we chose to wait and see. to clean up the scar tissue so that flow could be reestablished. Emmalyn underwent her third decompression on November 2nd, 2015. She sailed through surgery and the surgeon came out to talk with my dad and me. She explained that Emmalyn’s future could be complicated as she was developing a lot of scar tissue and that would make things more complex because it could continue to block the flow. The pain after these surgeries is something, they don’t prepare you for and after this surgery, it was worse than the last two. She came out swinging and hated everything. They got her pain under control, but it seemed like more pain medication was needed this time to keep it that way. This time, she spent four days in the hospital before returning home.
to clean up the scar tissue so that flow could be reestablished. Emmalyn underwent her third decompression on November 2nd, 2015. She sailed through surgery and the surgeon came out to talk with my dad and me. She explained that Emmalyn’s future could be complicated as she was developing a lot of scar tissue and that would make things more complex because it could continue to block the flow. The pain after these surgeries is something, they don’t prepare you for and after this surgery, it was worse than the last two. She came out swinging and hated everything. They got her pain under control, but it seemed like more pain medication was needed this time to keep it that way. This time, she spent four days in the hospital before returning home. Once again, her headaches and leg pain continued, but she was able to be upright again. In the middle of February, the back of her head became squishy again and her headaches started to get worse when upright. I called her neurosurgeon, and as always, more imaging was ordered, and as I suspected, her pseudomeningocele was back again. She delayed surgery as she wanted to do some research. So, Emmalyn laid down for most of a month. On March 31, we returned to the hospital for her sixth surgery. She went in and did the repair and placed an EVD drain, to check the pressure and drain CSF fluid. The drain was placed for a week, and it was the happiest and pain-free I had seen Emmalyn in over two years. Her pressures were all above 28, which meant high pressure. She made the decision that a VP shunt needed to be placed. Emmalyn went in for her seventh surgery on April 6th. Her Neurosurgeon came out and talked to me and my parents, she let me know that if this patch was to blow and another pseudomeningocele was to appear that at this point she wouldn’t know what to do next, that Emmalyn was too complex for her. I wanted to cry in fear for the first time. My dad said then what, whatever it was we would make it happen. Thank God for my dad, my rock. She said that she would refer us to a specialist she knew of in NYC. I prayed right there this night for god to take care of my little girl and heal her. After she woke up, the pain wasn’t as bad. Shunt placement seemed to be much easier than decompression. She stayed for two more days and was released to return home.
Once again, her headaches and leg pain continued, but she was able to be upright again. In the middle of February, the back of her head became squishy again and her headaches started to get worse when upright. I called her neurosurgeon, and as always, more imaging was ordered, and as I suspected, her pseudomeningocele was back again. She delayed surgery as she wanted to do some research. So, Emmalyn laid down for most of a month. On March 31, we returned to the hospital for her sixth surgery. She went in and did the repair and placed an EVD drain, to check the pressure and drain CSF fluid. The drain was placed for a week, and it was the happiest and pain-free I had seen Emmalyn in over two years. Her pressures were all above 28, which meant high pressure. She made the decision that a VP shunt needed to be placed. Emmalyn went in for her seventh surgery on April 6th. Her Neurosurgeon came out and talked to me and my parents, she let me know that if this patch was to blow and another pseudomeningocele was to appear that at this point she wouldn’t know what to do next, that Emmalyn was too complex for her. I wanted to cry in fear for the first time. My dad said then what, whatever it was we would make it happen. Thank God for my dad, my rock. She said that she would refer us to a specialist she knew of in NYC. I prayed right there this night for god to take care of my little girl and heal her. After she woke up, the pain wasn’t as bad. Shunt placement seemed to be much easier than decompression. She stayed for two more days and was released to return home.
 We returned to NYC at the end of the month and she went back into her first surgery of two on March 22, 2017. In the first surgery, he placed an EVD drain to drain CSF and to check pressures again. Her pressures were normal but on the higher size so he proceeded to surgery number two on March 29th. He removed the EVD drain and placed the new no valve shunt and the anti-siphoning device that could be changed when needed. It was a very painful surgery for Emmalyn as the placement of the anti-siphoning device was behind her ear in a very tender spot, and he also let me know she was the first child he had ever placed this in. She had recovered and returned home. Her headaches continued.
We returned to NYC at the end of the month and she went back into her first surgery of two on March 22, 2017. In the first surgery, he placed an EVD drain to drain CSF and to check pressures again. Her pressures were normal but on the higher size so he proceeded to surgery number two on March 29th. He removed the EVD drain and placed the new no valve shunt and the anti-siphoning device that could be changed when needed. It was a very painful surgery for Emmalyn as the placement of the anti-siphoning device was behind her ear in a very tender spot, and he also let me know she was the first child he had ever placed this in. She had recovered and returned home. Her headaches continued. We returned to Illinois. Her symptoms continued to be debilitating. I emailed him at least five times a week for answers and he quit answering. So, I called his office and they would set up phone call appointments that he never kept. All attempts to contact him were ignored for three long months, while our eight-year-old Emmalyn suffered. Until the day I emailed his college about the problems she was having, asking, begging for anyone to give us a second opinion, and what do you know he called me ten minutes later. He promised he would come up with a plan, and said he thought she needed pain management as everything surgical was stable. After a week of hearing nothing, I emailed him one last time. Asking him to open the back of her head and check for a leak, if there wasn’t one, I would concede to pain management. His office called the next day to set up surgery.
We returned to Illinois. Her symptoms continued to be debilitating. I emailed him at least five times a week for answers and he quit answering. So, I called his office and they would set up phone call appointments that he never kept. All attempts to contact him were ignored for three long months, while our eight-year-old Emmalyn suffered. Until the day I emailed his college about the problems she was having, asking, begging for anyone to give us a second opinion, and what do you know he called me ten minutes later. He promised he would come up with a plan, and said he thought she needed pain management as everything surgical was stable. After a week of hearing nothing, I emailed him one last time. Asking him to open the back of her head and check for a leak, if there wasn’t one, I would concede to pain management. His office called the next day to set up surgery. We returned home and as always headaches and leg pain had continued. We returned to NYC for post-op and imaging at the beginning of March. All imaging was done, and no leaks were found in the back of the head, but they noticed a “kink” in her brainstem and that her two syrinxes continued to be large. Her neurosurgeon believed everything was stable in her brain, even though the thoughts of CCI were still there. He began to focus on her spine. He sent her for a prone MRI (where she was laying on her stomach), and her surgeon said that she did not look tethered, and we were put back in the “wait and see” category.
We returned home and as always headaches and leg pain had continued. We returned to NYC for post-op and imaging at the beginning of March. All imaging was done, and no leaks were found in the back of the head, but they noticed a “kink” in her brainstem and that her two syrinxes continued to be large. Her neurosurgeon believed everything was stable in her brain, even though the thoughts of CCI were still there. He began to focus on her spine. He sent her for a prone MRI (where she was laying on her stomach), and her surgeon said that she did not look tethered, and we were put back in the “wait and see” category. The weekend after we returned home Emmalyn started complaining of a bad headache and stated that she heard a cracking noise in her head, and her head felt wobbly. I immediately emailed the two neurosurgeons. The plan was to get a CT on Monday. We found out the donor bone in her fusion had broken. The plan was to put her back in the cervical collar for it to heal. In just a few days of being in the cervical collar, the headaches were horrible, and her incision opened and looked infected. After talking with the neurosurgeons and talking with Emmalyn it was decided to return to NYC to have the top part of her fusion back in. On November 5th she went back in the OR once again to have the top part of the fusion put back in place. It was then that we learned just how extensive the infection had been, and our nightmare battling it began. After fusion surgery, she was placed back in the collar and the plastic surgeon that closed her stated that part of her incision had a blackness to it and needed to be revised and would have to be back in the OR in two weeks for revision. After the revision the infection returned. They put her on antibiotics and sent us home right before Christmas, after eight weeks in the city. Emmalyn’s headaches continued and did not get better, but the incision started to look better. Her round of antibiotics ended, and her incision opened again, so I sent pictures to her plastic surgeon and he wanted us back to NYC as soon as possible. We returned on January 2nd, 2019. We saw plastic surgery, infectious disease, and neurosurgery. Infectious disease was concerned that her hardware was infected, but neurosurgery said it wasn’t. After three weeks in the city, it was decided to take her into the OR and take the infected part off and see how deep it went. It was determined to be superficial, but they decided to keep her on the antibiotics. Her headaches continued to be bad, so the decision was made to keep her in NYC for the next month to monitor her. Her incision healed well on the antibiotics, so they discontinued the antibiotics. On February 27th she was taken into the OR for another ICP bolt, to check to see if high pressure returned. When upright her pressures were at 0 to -5 and laying down, they went as high as 8. Our neurosurgeon let us know that her pressures were normal, and a shunt would not help. After the surgery was done and we were discharged her incision opened, yet again. We went for her post-op visit with the neurosurgeon and he took one look and said her hardware had to be infected and needed to be removed. After speaking with her fusion surgeon, he stated there was no way we should be removing the hardware so soon, as she was not fused. So, they decided to take her in the OR and do a complete washout and cultures and put her on antibiotics indefinitely until the hardware could be removed. On March 11th she was taken into the OR once again and had a complete wash out with antibiotics. After the cultures returned with no answers, her infectious disease doctor put her on Cefadroxil 500mg twice daily until the hardware could be safely removed. After three months in the city, we finally returned home.
The weekend after we returned home Emmalyn started complaining of a bad headache and stated that she heard a cracking noise in her head, and her head felt wobbly. I immediately emailed the two neurosurgeons. The plan was to get a CT on Monday. We found out the donor bone in her fusion had broken. The plan was to put her back in the cervical collar for it to heal. In just a few days of being in the cervical collar, the headaches were horrible, and her incision opened and looked infected. After talking with the neurosurgeons and talking with Emmalyn it was decided to return to NYC to have the top part of her fusion back in. On November 5th she went back in the OR once again to have the top part of the fusion put back in place. It was then that we learned just how extensive the infection had been, and our nightmare battling it began. After fusion surgery, she was placed back in the collar and the plastic surgeon that closed her stated that part of her incision had a blackness to it and needed to be revised and would have to be back in the OR in two weeks for revision. After the revision the infection returned. They put her on antibiotics and sent us home right before Christmas, after eight weeks in the city. Emmalyn’s headaches continued and did not get better, but the incision started to look better. Her round of antibiotics ended, and her incision opened again, so I sent pictures to her plastic surgeon and he wanted us back to NYC as soon as possible. We returned on January 2nd, 2019. We saw plastic surgery, infectious disease, and neurosurgery. Infectious disease was concerned that her hardware was infected, but neurosurgery said it wasn’t. After three weeks in the city, it was decided to take her into the OR and take the infected part off and see how deep it went. It was determined to be superficial, but they decided to keep her on the antibiotics. Her headaches continued to be bad, so the decision was made to keep her in NYC for the next month to monitor her. Her incision healed well on the antibiotics, so they discontinued the antibiotics. On February 27th she was taken into the OR for another ICP bolt, to check to see if high pressure returned. When upright her pressures were at 0 to -5 and laying down, they went as high as 8. Our neurosurgeon let us know that her pressures were normal, and a shunt would not help. After the surgery was done and we were discharged her incision opened, yet again. We went for her post-op visit with the neurosurgeon and he took one look and said her hardware had to be infected and needed to be removed. After speaking with her fusion surgeon, he stated there was no way we should be removing the hardware so soon, as she was not fused. So, they decided to take her in the OR and do a complete washout and cultures and put her on antibiotics indefinitely until the hardware could be removed. On March 11th she was taken into the OR once again and had a complete wash out with antibiotics. After the cultures returned with no answers, her infectious disease doctor put her on Cefadroxil 500mg twice daily until the hardware could be safely removed. After three months in the city, we finally returned home. Emmalyn’s headaches continued as always. It had been her way of life for seven years. Now the new symptom of nausea started and never left. We returned in May to have her hardware removed. After it was removed her upright headaches came back strong, but her incision healed perfectly. We were there for another six weeks after surgery to be monitored and because of the low-pressure headaches that I knew all too well. I asked our neurosurgeon for a CT myelogram and he refused, saying he “still believed she had instability issues and there was definitely not a leak.” After going back and forth with him for a long time he refused to listen. I decided it was time for a second opinion. I reached out to another specialist and he had many questions and agreed to see her. I let her neurosurgeon know that because all he was willing to do is have her see pain management, we were headed for a second opinion. We left NYC and didn’t look back.
Emmalyn’s headaches continued as always. It had been her way of life for seven years. Now the new symptom of nausea started and never left. We returned in May to have her hardware removed. After it was removed her upright headaches came back strong, but her incision healed perfectly. We were there for another six weeks after surgery to be monitored and because of the low-pressure headaches that I knew all too well. I asked our neurosurgeon for a CT myelogram and he refused, saying he “still believed she had instability issues and there was definitely not a leak.” After going back and forth with him for a long time he refused to listen. I decided it was time for a second opinion. I reached out to another specialist and he had many questions and agreed to see her. I let her neurosurgeon know that because all he was willing to do is have her see pain management, we were headed for a second opinion. We left NYC and didn’t look back. California in September, where we met with a pain team and physical therapy. It was decided she needed a CT Myelogram as they were convinced there was a leak somewhere. After the Myelogram, we met with her neurosurgeon and it was determined Emmalyn had a leak at L1 in her lumbar spine. He recommended an epidural blood patch to repair the leak. We received a call from the pain team that the leak specialist agreed. We returned to sunny California on October 8, 2019, for her blood patch on October 9, 2019. On October 9th Emmalyn went into the OR for her blood patch. She had two blood patches placed due to the presence of scar tissue at her L1 and L2 from her tethered cord surgery. They placed one there but also did a second patch coming up from her tailbone to make sure that it would seal. She struggled for a few days in the hospital with rebound high-pressure, so her neurosurgeon put her on Diamox until we could figure out her new normal.
California in September, where we met with a pain team and physical therapy. It was decided she needed a CT Myelogram as they were convinced there was a leak somewhere. After the Myelogram, we met with her neurosurgeon and it was determined Emmalyn had a leak at L1 in her lumbar spine. He recommended an epidural blood patch to repair the leak. We received a call from the pain team that the leak specialist agreed. We returned to sunny California on October 8, 2019, for her blood patch on October 9, 2019. On October 9th Emmalyn went into the OR for her blood patch. She had two blood patches placed due to the presence of scar tissue at her L1 and L2 from her tethered cord surgery. They placed one there but also did a second patch coming up from her tailbone to make sure that it would seal. She struggled for a few days in the hospital with rebound high-pressure, so her neurosurgeon put her on Diamox until we could figure out her new normal.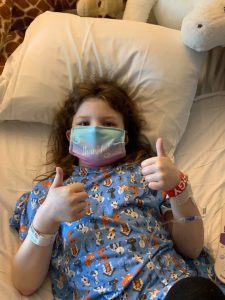 After the fifth patch, the doctors had serious discussions about what was next. Emmalyn’s headaches when upright were worse than they have ever been. After a lot of discussions, it was decided for Emmalyn to return to California on April 1st for another CT Myelogram (to check for remaining spinal leaks) with a Lumbar Puncture (to check her opening pressures), and surgical repair if necessary. The onslaught of COVID-19 hit. With so much unknown, we decided it would be safer to drive to California, rather than flying. Emmalyn and I rented a vehicle and hit the road on March 26th. We didn’t stop much and tried to do two states a day. The ride was a hard one on Emmalyn and the headaches were horrible, but we arrived in California on March 28th. Her Lumbar Puncture revealed that her opening pressure was twenty-four, which is a little on the high side, and not low like they expected. To make it even more confusing, the CT myelogram revealed a small leak still in the lumbar spine. The decision was made to do an EVD drain to drain CSF and recheck her pressures, to address the high-pressure issue first. On April 1st she was admitted for an EVD drain placement for seventy-two hours. She was put in the PICU (Pediatrics Intensive Care Unit) and at first, things weren’t improving at all. They dialed up the drain and as it was draining her headache began to improve by the last day her headache was at a two-out-of-ten, something we haven’t seen in an awfully long time. It was so great to see a genuine smile on Emmalyn. They removed the drain on Saturday afternoon, and she was discharged to the Ronald McDonald House, where we were staying. By Monday, her upright head pain returned with a vengeance. The decision was made to place a VP (ventriculoperitoneal) shunt with a Certas Programmable (adjustable) Valve.
After the fifth patch, the doctors had serious discussions about what was next. Emmalyn’s headaches when upright were worse than they have ever been. After a lot of discussions, it was decided for Emmalyn to return to California on April 1st for another CT Myelogram (to check for remaining spinal leaks) with a Lumbar Puncture (to check her opening pressures), and surgical repair if necessary. The onslaught of COVID-19 hit. With so much unknown, we decided it would be safer to drive to California, rather than flying. Emmalyn and I rented a vehicle and hit the road on March 26th. We didn’t stop much and tried to do two states a day. The ride was a hard one on Emmalyn and the headaches were horrible, but we arrived in California on March 28th. Her Lumbar Puncture revealed that her opening pressure was twenty-four, which is a little on the high side, and not low like they expected. To make it even more confusing, the CT myelogram revealed a small leak still in the lumbar spine. The decision was made to do an EVD drain to drain CSF and recheck her pressures, to address the high-pressure issue first. On April 1st she was admitted for an EVD drain placement for seventy-two hours. She was put in the PICU (Pediatrics Intensive Care Unit) and at first, things weren’t improving at all. They dialed up the drain and as it was draining her headache began to improve by the last day her headache was at a two-out-of-ten, something we haven’t seen in an awfully long time. It was so great to see a genuine smile on Emmalyn. They removed the drain on Saturday afternoon, and she was discharged to the Ronald McDonald House, where we were staying. By Monday, her upright head pain returned with a vengeance. The decision was made to place a VP (ventriculoperitoneal) shunt with a Certas Programmable (adjustable) Valve. Emmalyn went in for her Cisternogram with a Lumbar Puncture to check her opening pressure (which was normal… so the high-pressure was no longer a factor due to the shunt). The Cisternogram is generally a forty-eight-hour series of tests – beginning with an initial CT, another three hours later, another after six hours, then twenty-four-hours, and finally one at forty-eight-hours to check everywhere for a leak. Emmalyn did great and after the twenty-four-hour test, they said they didn’t need to do the next one. After a round-table discussion of doctors regarding the results of the test, it showed that Emmalyn had a leak at L4-5, and this time, they wanted to surgically repair it. On May 13th we went in for Emmalyn’s 38th surgery. Due to her constant leg pain, they also decided to do an ultrasound of her spine while in there to check her Tethered Cord area. She went in for surgery and four-and-a-half hours later the surgeon was out to speak with me. He found the leak and was able to repair it and upon the ultrasound of the spine, found that her spinal cord was complexly tethered again, stating “it was in a ball and he had to untether it.” He let me know that her EDS is severe and that her scar tissue is massive, so he went back in to try and repair all that he could.
Emmalyn went in for her Cisternogram with a Lumbar Puncture to check her opening pressure (which was normal… so the high-pressure was no longer a factor due to the shunt). The Cisternogram is generally a forty-eight-hour series of tests – beginning with an initial CT, another three hours later, another after six hours, then twenty-four-hours, and finally one at forty-eight-hours to check everywhere for a leak. Emmalyn did great and after the twenty-four-hour test, they said they didn’t need to do the next one. After a round-table discussion of doctors regarding the results of the test, it showed that Emmalyn had a leak at L4-5, and this time, they wanted to surgically repair it. On May 13th we went in for Emmalyn’s 38th surgery. Due to her constant leg pain, they also decided to do an ultrasound of her spine while in there to check her Tethered Cord area. She went in for surgery and four-and-a-half hours later the surgeon was out to speak with me. He found the leak and was able to repair it and upon the ultrasound of the spine, found that her spinal cord was complexly tethered again, stating “it was in a ball and he had to untether it.” He let me know that her EDS is severe and that her scar tissue is massive, so he went back in to try and repair all that he could. the resident and told him, “No, none of this is making me better it is making me worse.” He was patient and kind and told her if we didn’t do surgery it would continue to get worse yet. With Emmalyn’s blessing, I signed the consent and they took her back into surgery the next morning. After three hours they came out and told me it was a seroma and it was taken care of. By the next day, Emmalyn was ready to get up and her back was feeling somewhat better, but she couldn’t walk again. At this point, we didn’t know how long she would need the walker. We were in the hospital for another five days and over the course, she improved walking with a walker and her back pain subsided, but her headache was back all the time, and laying down wasn’t taking it away. We stayed in California until June 9th, where at this time Emmalyn was back walking on her own, another MRI was performed to check the seroma and it had fully dissipated, but her headaches were still 10/10 and even Dilaudid didn’t help. It was decided it was time to go home and give her a break from surgeries and time to heal, so Emmalyn and I hit the road. We decided to take a long route home to see friends and the Grand Canyon. (Since this has been such a long battle for all of us, I try to find ways to break the monotony of it all whenever I can if she’s up to it.) On day three of the drive (after seeing the Canyon), we stopped to rest and visit a friend, but Emmalyn was in so much pain, she was in tears and said she couldn’t continue with the drive. We had a carload of stuff, so the decision was made to pack everything in boxes and ship them, buy plane tickets out of Denver and fly home. Flights for Emmalyn are horrible, the pressure makes her headaches so much worse.
the resident and told him, “No, none of this is making me better it is making me worse.” He was patient and kind and told her if we didn’t do surgery it would continue to get worse yet. With Emmalyn’s blessing, I signed the consent and they took her back into surgery the next morning. After three hours they came out and told me it was a seroma and it was taken care of. By the next day, Emmalyn was ready to get up and her back was feeling somewhat better, but she couldn’t walk again. At this point, we didn’t know how long she would need the walker. We were in the hospital for another five days and over the course, she improved walking with a walker and her back pain subsided, but her headache was back all the time, and laying down wasn’t taking it away. We stayed in California until June 9th, where at this time Emmalyn was back walking on her own, another MRI was performed to check the seroma and it had fully dissipated, but her headaches were still 10/10 and even Dilaudid didn’t help. It was decided it was time to go home and give her a break from surgeries and time to heal, so Emmalyn and I hit the road. We decided to take a long route home to see friends and the Grand Canyon. (Since this has been such a long battle for all of us, I try to find ways to break the monotony of it all whenever I can if she’s up to it.) On day three of the drive (after seeing the Canyon), we stopped to rest and visit a friend, but Emmalyn was in so much pain, she was in tears and said she couldn’t continue with the drive. We had a carload of stuff, so the decision was made to pack everything in boxes and ship them, buy plane tickets out of Denver and fly home. Flights for Emmalyn are horrible, the pressure makes her headaches so much worse. The road with EDS, Chiari Malformation, CSF leaks, Tethered Cord Syndrome, Craniocervical Instability, and all the comorbids she’s faced, is such a long road for anyone that has it, but don’t give up, because the right surgeon or doctor will come along and hopefully be able to help make it better! Emmalyn’s story has been long and hard, and more than any little girl should have to endure. It’s impossible to go through forty surgeries in the eight years of her now eleven-year life and have a short story to tell. She’s stronger than any child should have to be and despite all the pain, she tries to maintain a cheerful disposition that brightens everyone’s day. Emmalyn wanted to share her story in hopes that it might help other children in their fight. We hope that her story will help other families understand the importance of advocating for their child, even if it means getting second/third opinions! Don’t believe everything your doctors say, research it for yourselves and push to get the medical care that your child deserves. If a surgeon is willing to do surgery but is unwilling to run tests, walk away, and get another opinion! Ask your child what they’re feeling and when they’re feeling it, as well as any changes that might be helping to relieve the pain (even if the relief is slight) because those are important details; and believe what they tell you even if you’re the only one that believes them. And beyond everything else, don’t give up and don’t give in! Fight it like you’re fighting for your child’s life because that is exactly what you’re doing – that is the fight!
The road with EDS, Chiari Malformation, CSF leaks, Tethered Cord Syndrome, Craniocervical Instability, and all the comorbids she’s faced, is such a long road for anyone that has it, but don’t give up, because the right surgeon or doctor will come along and hopefully be able to help make it better! Emmalyn’s story has been long and hard, and more than any little girl should have to endure. It’s impossible to go through forty surgeries in the eight years of her now eleven-year life and have a short story to tell. She’s stronger than any child should have to be and despite all the pain, she tries to maintain a cheerful disposition that brightens everyone’s day. Emmalyn wanted to share her story in hopes that it might help other children in their fight. We hope that her story will help other families understand the importance of advocating for their child, even if it means getting second/third opinions! Don’t believe everything your doctors say, research it for yourselves and push to get the medical care that your child deserves. If a surgeon is willing to do surgery but is unwilling to run tests, walk away, and get another opinion! Ask your child what they’re feeling and when they’re feeling it, as well as any changes that might be helping to relieve the pain (even if the relief is slight) because those are important details; and believe what they tell you even if you’re the only one that believes them. And beyond everything else, don’t give up and don’t give in! Fight it like you’re fighting for your child’s life because that is exactly what you’re doing – that is the fight!
 “But you look so good” is what people usually say when they find out that I struggle with debilitating chronic illnesses. It is true- I wear fashionable clothes, I do my hair, I put on makeup and I have a smile on my face. Underneath it all though, is someone who is trying to live her best life with the cards she was dealt with. I grew up in southern India and none of my family members knew what Chiari malformation was. It wasn’t until I came to the United States, had a baby and hit a complete rock bottom that I found out that a condition called Chiari even existed.
“But you look so good” is what people usually say when they find out that I struggle with debilitating chronic illnesses. It is true- I wear fashionable clothes, I do my hair, I put on makeup and I have a smile on my face. Underneath it all though, is someone who is trying to live her best life with the cards she was dealt with. I grew up in southern India and none of my family members knew what Chiari malformation was. It wasn’t until I came to the United States, had a baby and hit a complete rock bottom that I found out that a condition called Chiari even existed. with that same narrative, I started questioning if it was all indeed in my mind and psychosomatic. I was starting to accept that living like that was going to be my new normal. I was training with my figure skating coach to be able to make to adult nationals. Skating gave me joy because it was an artistic sport that I could distract myself with. But eventually, the pain took that joy away from me.
with that same narrative, I started questioning if it was all indeed in my mind and psychosomatic. I was starting to accept that living like that was going to be my new normal. I was training with my figure skating coach to be able to make to adult nationals. Skating gave me joy because it was an artistic sport that I could distract myself with. But eventually, the pain took that joy away from me. From the diagnosis of Chiari 1.5 to surgery was about 3 weeks. I liked my surgeon and the care team, so I was comfortable with the surgery. Recovery was long and painful though. I had meningitis twice after the surgery, developed chronic migraines in addition to trigeminal and occipital neuralgia. The diagnosis of central sleep apnea, MCAS and EDS came a year later. My brain stem was traumatized massively. I had to go to vestibular physical rehabilitation therapy to fully walk independently again. A year after my Chiari decompression, I had the Nissen Fundoplication to fix my esophagus. Four years past surgery, I am still recovering and learning how to manage my conditions. My care team now consists of – Anesthesiologist, Physiatrist, Neurologist, Pulmonologist, Gastroenterologist, ENT doctor, Massage Therapists, and Mental Health Counselors in addition to my close family. A huge part of learning how to manage these conditions has been figuring out what my physical limitations are and listening to my body cues. It has taken a long time to learn that it is ok to say no and that it is ok to have a LOT of mental energy but have little to no capacity to do things physically. I gave up figure skating because that kind of physical activity was causing me extreme pain. I get intense urges to skate every now and then which I give into occasionally but as the years have gone by, I am much better at gauging the pain and deciding not to do it. Loud sounds and bright lights trigger a lot of pain now, so I am better about avoiding places that I know are noisy and overwhelming. I have found peace in hiking through the wonderful trails of the pacific northwest. I have cut down on social commitments to prioritize my health over anything else. Some weekends, I do nothing except sleep all day… I have had to learn that that is OK. My husband has been a huge support and my pillar to lean on for the 11 years that we have been married. If I am tempted to do something against my better judgment, he reminds me to know my limitations. I have made peace with the fact that some people might find it impossible to hard to understand what living with Chiari and the comorbid conditions is like and that I cannot control how other people see it. My job has been a stable and joyful part of my life, but it took me a long time to accept that too since my original goal was to go to medical school. I realized my personal limitation about not being able to make it through medical residency. I want to let everyone know that there is hope at the other end of the tunnel… even though it is not in the form of a cure.
From the diagnosis of Chiari 1.5 to surgery was about 3 weeks. I liked my surgeon and the care team, so I was comfortable with the surgery. Recovery was long and painful though. I had meningitis twice after the surgery, developed chronic migraines in addition to trigeminal and occipital neuralgia. The diagnosis of central sleep apnea, MCAS and EDS came a year later. My brain stem was traumatized massively. I had to go to vestibular physical rehabilitation therapy to fully walk independently again. A year after my Chiari decompression, I had the Nissen Fundoplication to fix my esophagus. Four years past surgery, I am still recovering and learning how to manage my conditions. My care team now consists of – Anesthesiologist, Physiatrist, Neurologist, Pulmonologist, Gastroenterologist, ENT doctor, Massage Therapists, and Mental Health Counselors in addition to my close family. A huge part of learning how to manage these conditions has been figuring out what my physical limitations are and listening to my body cues. It has taken a long time to learn that it is ok to say no and that it is ok to have a LOT of mental energy but have little to no capacity to do things physically. I gave up figure skating because that kind of physical activity was causing me extreme pain. I get intense urges to skate every now and then which I give into occasionally but as the years have gone by, I am much better at gauging the pain and deciding not to do it. Loud sounds and bright lights trigger a lot of pain now, so I am better about avoiding places that I know are noisy and overwhelming. I have found peace in hiking through the wonderful trails of the pacific northwest. I have cut down on social commitments to prioritize my health over anything else. Some weekends, I do nothing except sleep all day… I have had to learn that that is OK. My husband has been a huge support and my pillar to lean on for the 11 years that we have been married. If I am tempted to do something against my better judgment, he reminds me to know my limitations. I have made peace with the fact that some people might find it impossible to hard to understand what living with Chiari and the comorbid conditions is like and that I cannot control how other people see it. My job has been a stable and joyful part of my life, but it took me a long time to accept that too since my original goal was to go to medical school. I realized my personal limitation about not being able to make it through medical residency. I want to let everyone know that there is hope at the other end of the tunnel… even though it is not in the form of a cure.![The Petra Johansson Story – A Chiari Warrior’s Journey [English Version]](https://dev.chiaribridges.org/wp-content/uploads/2019/11/Petra-Now2.jpg)
 It was spring 2017 and I was the happiest gal in the world. We had planned and longed for years and we were finally becoming a family. I could not have been happier. At that time, I was used to getting headaches when I coughed or sneezed, but I figured this happened to everyone. I would never have thought that something was wrong, but all of a sudden I started getting real headaches and I went to the doctor’s office. They said that it was just the pregnancy and that I didn’t need to worry so I went on with my life. However, the symptoms were escalating fast and I was losing my balance, strength, and coordination, and I had major issues with remembering and focusing. When I finally went to the doctor again, they sent me straight to the ER to get an MRI to rule out a stroke.
It was spring 2017 and I was the happiest gal in the world. We had planned and longed for years and we were finally becoming a family. I could not have been happier. At that time, I was used to getting headaches when I coughed or sneezed, but I figured this happened to everyone. I would never have thought that something was wrong, but all of a sudden I started getting real headaches and I went to the doctor’s office. They said that it was just the pregnancy and that I didn’t need to worry so I went on with my life. However, the symptoms were escalating fast and I was losing my balance, strength, and coordination, and I had major issues with remembering and focusing. When I finally went to the doctor again, they sent me straight to the ER to get an MRI to rule out a stroke. The next day the head of the department came to see me and told me that my cerebellum was protruding 13 mm from my skull and that they would have wanted me to have an operation immediately, but because of the baby – they would have to wait. Outside my hospital window, the world was getting ready for summer and the calendars now read, ”June 2017.”
The next day the head of the department came to see me and told me that my cerebellum was protruding 13 mm from my skull and that they would have wanted me to have an operation immediately, but because of the baby – they would have to wait. Outside my hospital window, the world was getting ready for summer and the calendars now read, ”June 2017.” what happened during that time. Dealing with the loss of our dream and my own illness was too much to bear, and I just shut down. The world was a cruel and harsh place.
what happened during that time. Dealing with the loss of our dream and my own illness was too much to bear, and I just shut down. The world was a cruel and harsh place. They removed 2.5 cm of my skull bone and 2 cm of the lamina from my atlas vertebra (C1) in March 2018. For two weeks I was fine until I developed chemical meningitis and was hospitalized. Well, fine is maybe an overstatement since they did forget to close my eye before the operation and it actually dried up and stuck to the operating table, scarring my cornea for life (yes, that is a thing). I waited and waited for that moment when I was supposed to feel good again. But it never came. I couldn’t lay down on my back or the back of my head without feeling like I was going to faint, my head pain was awful and I had several neurological symptoms. The doctors tried different medicines and painkillers but nothing worked or it gave me bizarre side effects. No matter what they tried, the pain wouldn’t subside.
They removed 2.5 cm of my skull bone and 2 cm of the lamina from my atlas vertebra (C1) in March 2018. For two weeks I was fine until I developed chemical meningitis and was hospitalized. Well, fine is maybe an overstatement since they did forget to close my eye before the operation and it actually dried up and stuck to the operating table, scarring my cornea for life (yes, that is a thing). I waited and waited for that moment when I was supposed to feel good again. But it never came. I couldn’t lay down on my back or the back of my head without feeling like I was going to faint, my head pain was awful and I had several neurological symptoms. The doctors tried different medicines and painkillers but nothing worked or it gave me bizarre side effects. No matter what they tried, the pain wouldn’t subside. Time was my worst enemy. I couldn’t believe how slowly it went by. February 2019 came and it was 11 months after I first lay on that table. I couldn’t manage the day to day life, I slept all through the day and I was in grave pain. If I tried laying on my back, I would pass out. My boyfriend took care of our house and me, and life was not a life worth living. Once again I tried contacting my doctor. This time I simply wrote a goodbye letter, I knew I was dying. He called me right away and told me that they were going to open me up again. There were still no indications in the images that something was wrong so they asked me to perform some tests before they would schedule me. I did neurological tests, a lumbar puncture, and a new MRI. I had to be put to sleep during the MRI because of my issues and the tests did show my pressure was a bit too high. However, the neurologist thought I had a couple of extra kilos for my height and attributed everything to me being slightly overweight. My second surgery was scheduled in April 2019.
Time was my worst enemy. I couldn’t believe how slowly it went by. February 2019 came and it was 11 months after I first lay on that table. I couldn’t manage the day to day life, I slept all through the day and I was in grave pain. If I tried laying on my back, I would pass out. My boyfriend took care of our house and me, and life was not a life worth living. Once again I tried contacting my doctor. This time I simply wrote a goodbye letter, I knew I was dying. He called me right away and told me that they were going to open me up again. There were still no indications in the images that something was wrong so they asked me to perform some tests before they would schedule me. I did neurological tests, a lumbar puncture, and a new MRI. I had to be put to sleep during the MRI because of my issues and the tests did show my pressure was a bit too high. However, the neurologist thought I had a couple of extra kilos for my height and attributed everything to me being slightly overweight. My second surgery was scheduled in April 2019. Nobody really knows what is wrong with me and how to handle it. I am a great enigma with my doctors and I can not trust anyone to be my advocate and do the research, so I do it myself. I’ve learned to ask tough questions and not give up and I have also learned to ask for help from people in my position. What are they doing and how can I apply that to my life. Without the community, I would be lost. I would not know what to do when I get to yet another doctor or nurse who asks, ”You have WHAT?” I don’t think I would have had the strength to keep on fighting if I didn’t know that I wasn’t alone. I am pretty sure nothing else can happen now that I haven’t already been through. I have more knowledge and experience, but I am also more worn out, exhausted and sometimes just jaded from having to constantly fight. To go through two major surgeries without any relief is not easy peasy. Sometimes it just sucks – I am supposed to get better from treatments, not worse. Right?
Nobody really knows what is wrong with me and how to handle it. I am a great enigma with my doctors and I can not trust anyone to be my advocate and do the research, so I do it myself. I’ve learned to ask tough questions and not give up and I have also learned to ask for help from people in my position. What are they doing and how can I apply that to my life. Without the community, I would be lost. I would not know what to do when I get to yet another doctor or nurse who asks, ”You have WHAT?” I don’t think I would have had the strength to keep on fighting if I didn’t know that I wasn’t alone. I am pretty sure nothing else can happen now that I haven’t already been through. I have more knowledge and experience, but I am also more worn out, exhausted and sometimes just jaded from having to constantly fight. To go through two major surgeries without any relief is not easy peasy. Sometimes it just sucks – I am supposed to get better from treatments, not worse. Right?
 When I first started getting hit with symptoms, I was a divorced, single mother of three amazing kids; responsible not only to provide for them but to see them through life, unscathed by life’s situations, and showing them that there was nothing that if they worked hard at something, nothing could hold them back. I had just started to expand in my career as a self-taught auto technician. I was a woman making a place for herself in an industry traditionally dominated by males. July 3, 2015, was the day that my life forever changed. I was brought to the hospital with stroke-like symptoms. I was having visual problems. I couldn’t walk or talk. I had no idea who I was or where I was. The whole right side of my body basically stopped working and the right side of my face was droopy. I was brought to the ER and before the doctor would even try to figure out what was wrong with me, he ordered a series of drug tests. I passed every test, so he finally admitted to me. Once on the neurology floor, more testing was done. They performed an MRI, MRA, EKG and told us that all results were normal. I later discovered that was not the case.
When I first started getting hit with symptoms, I was a divorced, single mother of three amazing kids; responsible not only to provide for them but to see them through life, unscathed by life’s situations, and showing them that there was nothing that if they worked hard at something, nothing could hold them back. I had just started to expand in my career as a self-taught auto technician. I was a woman making a place for herself in an industry traditionally dominated by males. July 3, 2015, was the day that my life forever changed. I was brought to the hospital with stroke-like symptoms. I was having visual problems. I couldn’t walk or talk. I had no idea who I was or where I was. The whole right side of my body basically stopped working and the right side of my face was droopy. I was brought to the ER and before the doctor would even try to figure out what was wrong with me, he ordered a series of drug tests. I passed every test, so he finally admitted to me. Once on the neurology floor, more testing was done. They performed an MRI, MRA, EKG and told us that all results were normal. I later discovered that was not the case. A few days later, I followed up with my PCP. She went over my MRI results with me and pointed out that they found a Chiari Malformation with a 19mm herniation of my cerebellar tonsils. She told me of changes in my white matter that the radiologist said needed to be “further evaluated” and referred me to my first neurologist, who I met within August. He ordered a visual evoked potential and an EEG. Both come back normal, so he diagnosed me with migraines, even after hearing my symptoms, which frustrates me even more as I know that it is not migraines causing these issues.
A few days later, I followed up with my PCP. She went over my MRI results with me and pointed out that they found a Chiari Malformation with a 19mm herniation of my cerebellar tonsils. She told me of changes in my white matter that the radiologist said needed to be “further evaluated” and referred me to my first neurologist, who I met within August. He ordered a visual evoked potential and an EEG. Both come back normal, so he diagnosed me with migraines, even after hearing my symptoms, which frustrates me even more as I know that it is not migraines causing these issues. During this care for MS, I kept having what they thought were MS relapses, roughly every three to four months. Each time they ordered new MRI images and treated me with high doses of IV steroids for five days in a row. Never once did this imaging ever show an actual MS-relapse or MS activity. I continually had issues with every medication that they put me on to help “try to delay the progression of the MS” (the MS that I never had). In November 2017 I started Ocrevus, which was just FDA approved that year. Around this time, I started having strange symptoms and thought them just to be side effects of the medication, not realizing that something else might be causing it all. I met with my neurologist before my second full dose and I told her everything that I was experiencing. We opted to take me off the Ocrevus and they repeated the MRI yet again. Again, the MRIs show absolutely nothing new for activity and she admits that she doesn’t know what to do for me. I am three years in at that point and never once have they seen any MS activity.
During this care for MS, I kept having what they thought were MS relapses, roughly every three to four months. Each time they ordered new MRI images and treated me with high doses of IV steroids for five days in a row. Never once did this imaging ever show an actual MS-relapse or MS activity. I continually had issues with every medication that they put me on to help “try to delay the progression of the MS” (the MS that I never had). In November 2017 I started Ocrevus, which was just FDA approved that year. Around this time, I started having strange symptoms and thought them just to be side effects of the medication, not realizing that something else might be causing it all. I met with my neurologist before my second full dose and I told her everything that I was experiencing. We opted to take me off the Ocrevus and they repeated the MRI yet again. Again, the MRIs show absolutely nothing new for activity and she admits that she doesn’t know what to do for me. I am three years in at that point and never once have they seen any MS activity. The last four years have been one hell of a ride when it comes to my health. My health problems have made it far more difficult to continue working on cars. As my symptoms wage war on my body, I am now forced to work on light duty and have been for the last two and a half years. I know that my days of working in a shop are coming to end as I just can’t handle the physical requirements of the job anymore. My quality of life in the last year alone has declined sharply. I used to be the energetic mom who could coach a sports team after working all day in the shop and still have the energy to keep up with the housework, now that is not the case. I manage to push on and get them to their activities, but I’m exhausted to the core. When this all began back in 2015 my kids were 8, 7, and 5. They are now 12, 11 and 9. At times I feel like I am a horrible mother because I miss the mom that I used to be. I miss the days when my kids weren’t worried about my health and when we could make plans with other families and keep them. I have lost so much of who I am thanks to the ignorance of some members of the medical community. I am losing faith in the medical profession in general. Male doctors have been the worst as I go through this journey, as women seem to have to first prove that it’s not psychosomatic before we’re worthy of being helped, even with imaging shows something to the contrary. When I present them with proven facts about Chiari Malformation, it still gets dismissed and it is extremely frustrating. The longer I go without receiving proper treatment, the more likely it becomes that some of this damage will become permanent and to me, that is not acceptable. I am fighting for my life and I will not back down until I receive the proper care, I can’t!
The last four years have been one hell of a ride when it comes to my health. My health problems have made it far more difficult to continue working on cars. As my symptoms wage war on my body, I am now forced to work on light duty and have been for the last two and a half years. I know that my days of working in a shop are coming to end as I just can’t handle the physical requirements of the job anymore. My quality of life in the last year alone has declined sharply. I used to be the energetic mom who could coach a sports team after working all day in the shop and still have the energy to keep up with the housework, now that is not the case. I manage to push on and get them to their activities, but I’m exhausted to the core. When this all began back in 2015 my kids were 8, 7, and 5. They are now 12, 11 and 9. At times I feel like I am a horrible mother because I miss the mom that I used to be. I miss the days when my kids weren’t worried about my health and when we could make plans with other families and keep them. I have lost so much of who I am thanks to the ignorance of some members of the medical community. I am losing faith in the medical profession in general. Male doctors have been the worst as I go through this journey, as women seem to have to first prove that it’s not psychosomatic before we’re worthy of being helped, even with imaging shows something to the contrary. When I present them with proven facts about Chiari Malformation, it still gets dismissed and it is extremely frustrating. The longer I go without receiving proper treatment, the more likely it becomes that some of this damage will become permanent and to me, that is not acceptable. I am fighting for my life and I will not back down until I receive the proper care, I can’t!
 I was what you would consider a “typical developing child” growing up, I did not have any health issues and was able to enjoy much of my childhood. My journey to finding answers in regard my health began at 15 years old, when I began rapidly losing my vision in my left eye. I dealt with severe headaches and the doctors struggled to draw a connection to my declining vision. I went from 20/20 vision to 20/400 in my right eye and 0 vision in my left. I was considered legally blind. I had to relearn how to navigate life with very little vision.
I was what you would consider a “typical developing child” growing up, I did not have any health issues and was able to enjoy much of my childhood. My journey to finding answers in regard my health began at 15 years old, when I began rapidly losing my vision in my left eye. I dealt with severe headaches and the doctors struggled to draw a connection to my declining vision. I went from 20/20 vision to 20/400 in my right eye and 0 vision in my left. I was considered legally blind. I had to relearn how to navigate life with very little vision. Fast forward a few years, I was told that a second decompression surgery was required, which I agreed to. It resulted in a rip in my dural patch causing a cerebral spinal fluid leak at the surgical site. After these two decompression and a CSF leak repair surgery, my vision had improved significantly yet I was worse off symptom wise than I was when I initially began noticing changes in my body. Sadly, I was told from my specialists that there was nothing more they could do for me. They referred me to the headache/face pain clinic. After many failed attempts at managing my pain with medications, my doctor mentioned that my symptoms resembled a spinal fluid leak and that there is a doctor who is navigating research and I should be evaluated.
Fast forward a few years, I was told that a second decompression surgery was required, which I agreed to. It resulted in a rip in my dural patch causing a cerebral spinal fluid leak at the surgical site. After these two decompression and a CSF leak repair surgery, my vision had improved significantly yet I was worse off symptom wise than I was when I initially began noticing changes in my body. Sadly, I was told from my specialists that there was nothing more they could do for me. They referred me to the headache/face pain clinic. After many failed attempts at managing my pain with medications, my doctor mentioned that my symptoms resembled a spinal fluid leak and that there is a doctor who is navigating research and I should be evaluated. contrast, CT , digital subtraction myelogram, MR myelogram, and the list goes on. After a few months of investigating we were able to confirm that I suffer from spontaneous intracranial hypotension, meaning that I have multiple leaks or suspicious areas in my spine, that happened spontaneously (without known trauma). My doctor mentioned that my Chiari diagnosis is what is classified as an Acquired Chiari Malformation.
contrast, CT , digital subtraction myelogram, MR myelogram, and the list goes on. After a few months of investigating we were able to confirm that I suffer from spontaneous intracranial hypotension, meaning that I have multiple leaks or suspicious areas in my spine, that happened spontaneously (without known trauma). My doctor mentioned that my Chiari diagnosis is what is classified as an Acquired Chiari Malformation.
 I had a rough journey with these conditions and I am sharing it to help show how complex we can be and how much we need the medical community to step it up a notch (or ten)! I grew up in Denmark, where I lived when I was diagnosed and had my first surgeries.
I had a rough journey with these conditions and I am sharing it to help show how complex we can be and how much we need the medical community to step it up a notch (or ten)! I grew up in Denmark, where I lived when I was diagnosed and had my first surgeries. Years passed by with various periods of severe pain flares, flares that felt nothing like the pains I had before. But no doctor was really believing me. I had a spontaneous collapsed lung a couple of times in this period and ended up with surgery for this (I woke up under this surgery which later also turned out to have a significance). At 25, one day I had a sudden and severe onset of symptoms – a pain in the back of my head feeling like two stabbing knives. This did not resolve and after several attempts with various medicines, that I only got sicker from, I finally saw a new rheumatologist whom again treated me with harsh accusations of laziness and psychological imbalance. I can assure you he was the one bringing on my tears that day, despite the extra severe pain I had been in for weeks. I was placed in the care of the hospital physios and after a while, it became clear to them that there was something really wrong and they got me to see another rheumatologist, who in turn took their word and referred me for an MRI. I had only just turned 26 when I was diagnosed with Chiari 1 Malformation and Syringomyelia – in my full spine.
Years passed by with various periods of severe pain flares, flares that felt nothing like the pains I had before. But no doctor was really believing me. I had a spontaneous collapsed lung a couple of times in this period and ended up with surgery for this (I woke up under this surgery which later also turned out to have a significance). At 25, one day I had a sudden and severe onset of symptoms – a pain in the back of my head feeling like two stabbing knives. This did not resolve and after several attempts with various medicines, that I only got sicker from, I finally saw a new rheumatologist whom again treated me with harsh accusations of laziness and psychological imbalance. I can assure you he was the one bringing on my tears that day, despite the extra severe pain I had been in for weeks. I was placed in the care of the hospital physios and after a while, it became clear to them that there was something really wrong and they got me to see another rheumatologist, who in turn took their word and referred me for an MRI. I had only just turned 26 when I was diagnosed with Chiari 1 Malformation and Syringomyelia – in my full spine. I did a bit of internet research as information in Danish was very sparse and realized there was a certain number of bad outcomes due to something called Ehlers-Danlos Syndrome, Retroflexed Odontoid and Basilar Invagination. I asked my neurosurgeon, who was supposed to be the best in Denmark at this point, about these things – he claimed I didn’t have any. However, he did agree to refer me for Ehlers-Danlos evaluation. Here I was told I did not have that either. However, I was bordering on a similar connective tissue disorder called Marfan Syndrome, which they still could not diagnose me with due to my heart and eyes not being faulty. I had my first decompression surgery in December 2006. It was rough. I reacted badly to anesthetics and to the morphine and I also lost a lot of spinal fluid. I could not raise myself up the first month which I thought was normal. Slowly, I got better, and imaging showed my syrinx shrinking. Two and a half years later, though, I started experiencing dizziness and nausea and though my first surgeon didn’t believe me, imaging finally showed a big collection of fluid outside my spinal cord originating from a hole in the duraplasty used to close after tonsillar cauterization at my first surgery. I tried talking to the surgeon about concerns of Klippel-Feil and instability, that I had read about, but they would not hear of it and said that for now they would just focus on this issue. So, this was repaired, and I moved to Spain with my boyfriend at the time. I was placed on a disability pension from Denmark and that enrolled me in the Spanish public healthcare. I did, however, in the meantime follow up on my concerns and contacted a specialist, who had written about the Klippel-Feil and Chiari connection, and he straight away stated I had some severe issues with my odontoid and needed it removed and my neck fused to my skull. My first meeting with a surgeon in Spanish health care came up and he just looked at my imaging two minutes then stated my problems were way bigger than Chiari and Syringomyelia. He also diagnosed a severe retroflexed odontoid and Basilar Invagination – so severe he had a hard time understanding how I could breathe, let alone walk. But given my reasonably good condition, he opted to postpone these surgeries as they are big and not without risks.
I did a bit of internet research as information in Danish was very sparse and realized there was a certain number of bad outcomes due to something called Ehlers-Danlos Syndrome, Retroflexed Odontoid and Basilar Invagination. I asked my neurosurgeon, who was supposed to be the best in Denmark at this point, about these things – he claimed I didn’t have any. However, he did agree to refer me for Ehlers-Danlos evaluation. Here I was told I did not have that either. However, I was bordering on a similar connective tissue disorder called Marfan Syndrome, which they still could not diagnose me with due to my heart and eyes not being faulty. I had my first decompression surgery in December 2006. It was rough. I reacted badly to anesthetics and to the morphine and I also lost a lot of spinal fluid. I could not raise myself up the first month which I thought was normal. Slowly, I got better, and imaging showed my syrinx shrinking. Two and a half years later, though, I started experiencing dizziness and nausea and though my first surgeon didn’t believe me, imaging finally showed a big collection of fluid outside my spinal cord originating from a hole in the duraplasty used to close after tonsillar cauterization at my first surgery. I tried talking to the surgeon about concerns of Klippel-Feil and instability, that I had read about, but they would not hear of it and said that for now they would just focus on this issue. So, this was repaired, and I moved to Spain with my boyfriend at the time. I was placed on a disability pension from Denmark and that enrolled me in the Spanish public healthcare. I did, however, in the meantime follow up on my concerns and contacted a specialist, who had written about the Klippel-Feil and Chiari connection, and he straight away stated I had some severe issues with my odontoid and needed it removed and my neck fused to my skull. My first meeting with a surgeon in Spanish health care came up and he just looked at my imaging two minutes then stated my problems were way bigger than Chiari and Syringomyelia. He also diagnosed a severe retroflexed odontoid and Basilar Invagination – so severe he had a hard time understanding how I could breathe, let alone walk. But given my reasonably good condition, he opted to postpone these surgeries as they are big and not without risks. A couple of years of enjoying the benefits the climate change gave me (and likely putting my head in the sand) went by but then I could no longer ignore the fact that I was getting worse. I was in a rough period with other matters of life, so it took a while before I realized I couldn’t escape the changes in my body. I started losing weight amongst other things and after a quick detour of fear of stomach cancer, I finally realized that everything that was going on was related to my brainstem compression. So, I went back to the neurosurgeon. He ordered some testing but before it could be done, I ended up admitted urgently after I stopped breathing one night. From here started a roller coaster. I didn’t feel right about their suggestions and the surgeon that was going to operate didn’t feel very secure himself even. I ended up getting transferred to a private hospital in Barcelona that calls themselves a “Chiari Institute.” Had I known what I do now, I would never have paid the fee for a filum release, but the doctor claimed this was what I needed and well… It was worth a shot in this urgent situation. He then sent me home, claiming I was cured. I didn’t feel right and breathing through the night was still a problem, so I started sending my imaging to experts around the world and working on getting referred to another hospital in Spain’s public health with higher expertise. All these experts claimed I wouldn’t have long to live unless I had this odontoid approached.
A couple of years of enjoying the benefits the climate change gave me (and likely putting my head in the sand) went by but then I could no longer ignore the fact that I was getting worse. I was in a rough period with other matters of life, so it took a while before I realized I couldn’t escape the changes in my body. I started losing weight amongst other things and after a quick detour of fear of stomach cancer, I finally realized that everything that was going on was related to my brainstem compression. So, I went back to the neurosurgeon. He ordered some testing but before it could be done, I ended up admitted urgently after I stopped breathing one night. From here started a roller coaster. I didn’t feel right about their suggestions and the surgeon that was going to operate didn’t feel very secure himself even. I ended up getting transferred to a private hospital in Barcelona that calls themselves a “Chiari Institute.” Had I known what I do now, I would never have paid the fee for a filum release, but the doctor claimed this was what I needed and well… It was worth a shot in this urgent situation. He then sent me home, claiming I was cured. I didn’t feel right and breathing through the night was still a problem, so I started sending my imaging to experts around the world and working on getting referred to another hospital in Spain’s public health with higher expertise. All these experts claimed I wouldn’t have long to live unless I had this odontoid approached. October 2016 I finally had a partial odontoidectomy and a fusion, which beyond doubt saved my life. It was a rough ride, for both me and the surgeons. They had to deal with complications related to my anatomy, to the mess the first surgeon in Denmark had left – he had indeed damaged my muscles more than I ever knew – and to the problems relating to the soft tissue. I do know they did a great job, but due to all the mistakes, how complicated my case was and is, I am unfortunately not done. I have ongoing issues and though some of these could have been avoided with the right approach from the beginning, some are just the way it is with these conditions.
October 2016 I finally had a partial odontoidectomy and a fusion, which beyond doubt saved my life. It was a rough ride, for both me and the surgeons. They had to deal with complications related to my anatomy, to the mess the first surgeon in Denmark had left – he had indeed damaged my muscles more than I ever knew – and to the problems relating to the soft tissue. I do know they did a great job, but due to all the mistakes, how complicated my case was and is, I am unfortunately not done. I have ongoing issues and though some of these could have been avoided with the right approach from the beginning, some are just the way it is with these conditions.![The Christopher Ellington Story – A Chiari Warrior’s Journey [Updated]](https://dev.chiaribridges.org/wp-content/uploads/2017/05/hosp1.jpg)


